From the Brink to a New Beginning: One Woman’s Journey Through Homelessness, Healing, and Hope
July 30, 2025
After nearly dying on the streets of Austin, 56-year-old Glenda “Gigi” Locke found strength, stability, and self-worth with help from Central Health’s medical respite and case management programs.
AUSTIN, Texas— For years, good things didn’t happen to Glenda Locke. That was the reality of a life of addiction, for 25 years of choices that led her to this point.
Then one day in May, that changed.
During an assisted treatment for addiction appointment at the Central Health Southeast Health & Wellness Center, the 56-year-old was faced with a startling realization: good things were possible.
“How do you feel about that?” the physician, Dr. John Weems, said.
“I’m scared,” Locke replied. “I’m scared because it’s been a long time since I’ve been a responsible adult. I’m still dealing with my wreckage.”
A little over a year earlier, Locke almost died on the streets of Austin, her kidneys failing. She was placed in a medically induced coma, then woke up in an intensive care unit surrounded by nurses and physicians, her body hooked up to a dialysis machine.

Now, inside the room facing the CommUnityCare doctor she had grown to admire, Locke was on the verge of something else entirely: permanent housing for the first time since her five-year homeless spell began in 2020.
“It’s a huge change,” Dr. Weems said. “You’ve survived so much.”
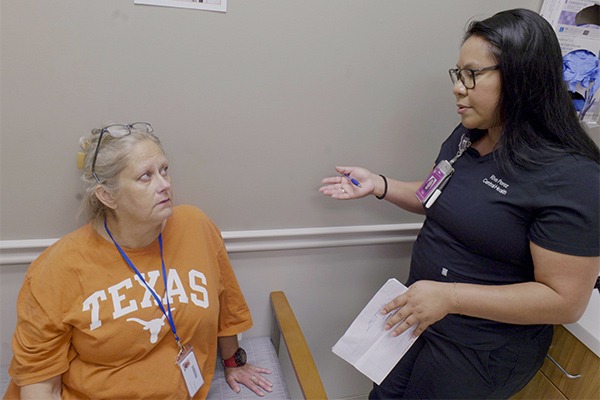
Central to that transformation was a bond Locke formed about a year earlier with Riva Perez, her Central Health case manager and community health worker (CHW), who gave her the confidence and autonomy to believe in herself again, urging her toward small steps—such as making, and then attending, medical appointments. Perez made a promise to her early on.
“I’ll be here until the end,” she said, referring to Locke’s search for permanent housing.
To help a person in need, a system must be in place. And for Locke, who needed those interventions, there were countless touch points connecting her to the outside world—physicians, nurses, CHWs, and case managers who entered her life when she was most in need.
First Interactions at New Entry
A person in need of care doesn’t always know where to go. Unhoused populations aren’t scouring the internet for the best hospitals as they battle addiction or a serious medical episode, so it’s up to the safety-net health systems to provide quality health care for those patients. Many times, people experiencing homelessness simply have no way to reach providers.
Locke’s world only extended as far as she could see, so once her life changed dramatically in March 2024, her routine changed instantly. First, the Central Health Transitions of Care team sent her to a skilled nursing facility (SNF), where she recovered under the care of a medical team including physicians and nurses.
A month later, she was housed in ‘A New Entry,’ a residential treatment program wherein Central Health’s medical respite team contracted out for beds. While it wasn’t a long-term housing solution, the program featured respite beds—temporary beds where patients can recover safely while receiving medical care—and comprehensive, around-the-clock support that addresses not just medical needs but also social services, mental health, and other aspects of a person’s wellbeing.
“The medical respite program gives individuals an opportunity for continued rest and recovery and connection to services after an acute illness,” said Dr. Audrey Kuang, Central Health’s co-director of high-risk populations. “Gigi is a great example of someone who needed additional time for rest after her hospital and nursing home stay. Respite gave her a chance to continue her recovery and stay engaged with her health team.”
This was where Locke first met Perez (along with registered nurse Laura Malone and social worker Dustin Wade). As a CHW in respite care, Perez and her partners helped Locke with her medications and made sure she was meeting the program’s requirements. But Locke also faced serious medical hurdles, such as stage 3 kidney disease and congenital heart failure.
By late July, Locke was discharged from the Central Health medical respite program and found a home at the Marshalling Yard, an expansive residential facility for Austin’s unhoused population near Austin-Bergstrom Airport.
Perez, meanwhile, transitioned into Central Health’s case management program. By August, the pair connected again.
Building Trust and Pushing Forward
Building trust with Locke didn’t come easy at first.
“She’s homeless this whole time, so she didn’t know who to trust,” Perez said. “She only knew that people had taken advantage of her.”
But Perez leaned on her near-instant connection with Perez and the pair eventually gave each other nicknames, with Locke calling her case manager “Honey,” while Perez learned to call Locke “Gigi.”
Perez reminded Locke that she was there to help her get housing. However, in November, after applying for Social Security and Disability Insurance (SSDI) for the first time, Locke experienced her first setback.
She was denied coverage.
The next two months, Locke faced hardship as she reverted to old patterns and sometimes refused to accept help. It placed Perez and her team in a difficult position.

“We contemplated letting her go from case management,” said Perez, who explained, “our rule is that the patient needs to work hard for this, and when they don’t, there’s little we can do.”
But, Perez said, “I really advocated for her, because I knew she could do it.”
As Perez championed for Locke, her patient eventually pushed forward and began to turn the corner with the help of a basic cell phone acquired through a local program, which ensured she could book and make appointments.
In January, Locke began connecting with the Central Health system—which includes CommUnityCare Health Centers and Sendero Health Plans—nearly every day, meeting with providers across various diagnostic services.
At the beginning of the year, she met Dr. Weems at the Southeast Health & Wellness Center. In their meetings, he would provide professional counsel and treatment. But what also built a sense of trust between the pair was his temperament, or the fact that he listened and provided a space free of judgement.
Locke’s journey also took her to a primary care provider with CommUnityCare and to nephrologist (kidney doctor) Dr. Michelle Lubetzky at the Rosewood-Zaragosa Health and Wellness Clinic. She received dental work at the CommUnityCare Chalmers Courts Health Center and went through the re-application of SSDI with the help of Central Health SOAR Case Manager Becca Cline. She also received behavioral health medical guidance from CommUnityCare Advanced Practice Provider of Psychiatry Danielle Sadeh.
From January to April 2025, Locke’s life began to transform.
“It’s about connecting people to resources.” – Lauren Galindo, the Central Health Operations Manager for Transitions of Care.
“I had 27 appointments in seven weeks,” said Locke, who was taking upwards of 26 pills per day at one point. “I had four appointments every week for six weeks, and then three last week.”
Another huge shift? Locke’s own image of herself.
When she was first discharged from the hospital in March 2024, her hair was matted and tangled, almost impossible to comb. A month later, while in respite with Perez and Malone, they took her to get a haircut. The pair eventually advised the barber to give Locke a buzz cut, because it was the only way her hair would grow back naturally.
By the following year, her blonde hair was long again, neatly tied back in a clip.
“Her willingness to go ahead,” Perez said, impressed.
A New Home
The tides turned quickly for Locke in 2025.
Initially, she had been denied SSDI, Perez said, due to “lack of evidence,” which meant that while it was recognized Locke needed the assistance, there was no way to quantify that fact without a list of medical diagnoses, and prescribed treatments and services.
Midway into the new year, however, with those evaluations logged and accounted for, a weight lifted. In the second application, Perez said, she wrote down every single diagnostic service Locke received, as well as every single specialty appointment and every medical provider that saw her.
Locke’s application was as solid as a rock. Perez called Locke to notify her when to pick up her phone.
“I was able to tell her, ‘Somebody is going to call you in two hours. Can you answer the phone?” Perez said.
Locke’s approved SSDI, which included a monthly stipend and enrollment into Medicaid, gave her resources she hadn’t had access to for 25 years.
An Even Bigger Win
When Perez learned Locke was approved for SSDI, she contacted Endeavors—the third-party organization that provides case management and crisis response at the Marshalling Yard—about the Cady Lofts, a 100-unit permanent housing community for individuals experiencing chronic homelessness.
The Ending Community Homeless Coalition (ECHO) facilitated the new lofts, and it had a coordinated entry process required by the U.S. Department of Housing and Urban Development. The apartments opened in April through SGI Ventures Inc. and the Austin Affordable Housing Corporation.
An application was submitted, and then approved, within days. Sitting at her work desk on a Friday morning, Perez received a call from Locke.
“She was crying with joy,” Perez said.

A Life Ahead for Glenda Locke
Locke moved into her fully furnished studio apartment in May, which features a walk-in closet, a standing shower, shelving for her clothes, a kitchen island, air conditioning, a bed to sleep in and a chair to rest her body and feet.
It was the culmination of over a year of work from Perez—and for that matter the Central Health system.
“She’s built skills to where she’s able to navigate life by herself now. I won’t be able to help her in the capacity that I was before, but if she ever needs me, I’m a call away. And I can guide her in the right direction.” – Riva Perez, Central Health Community Health Worker and Transitions of Care Case Manager
Locke represented the fourth patient she successfully led to permanent housing. But her journey from homelessness to having a home of her own also triggered that promise kept for Perez.
“The end,” as she put it.
With case management success and permanent housing comes the next phase of the journey: the transitional 30 days between the old and new providers. Locke will receive a new case management team with Medicaid, which means Perez’s work with her will end.
It’s a poignant reminder of the work she does every day, with every one of her 18 other patients across the Central Health system—that all good outcomes mean the end of one phase of life, and the start of a new.
“She’s built skills to where she’s able to navigate life by herself now,” Perez said of Locke. “I won’t be able to help her in the capacity that I was before, but if she ever needs me, I’m a call away. And I can guide her in the right direction.”
While Locke knows the road ahead won’t be simple, she says she remains hopeful for the future.
“I have not been a regular person in over 25 years,” Locke said. “I don’t have anybody to fall back on anymore. Riva helped me learn to be an adult.”

A good day is one that includes all the normalcies of daily life, and for Locke, that’s something she’s been striving to achieve for a long time.
“It’s something as small as going to the doctor, going to the store, making calls for my prescriptions,” she said. “I haven’t done that in years, so I’m hoping to grow as a person, branch out.”